Interview: Extensive experience in orthopaedic surgery at Helios Krefeld
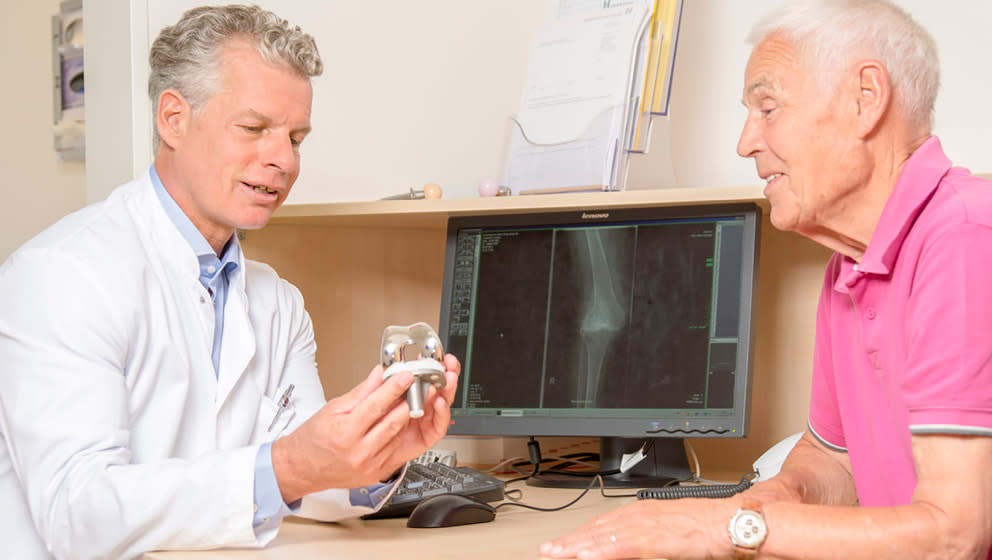
FFToday we are talking to Prof. Dr. Med. Clayton Kraft, head of the clinic for orthopedics, trauma, and hand surgery at Helios Hospital Krefeld, about orthopedic procedures as well as modern and traditional approaches in endoprosthetic surgery.
I’ve been interested in medicine and everything related to it since my childhood. It started with books on medicine. They would completely engross me. Just like any other child interested in the topic, I would watch doctors on TV and in films. Later on, it turned into my desire to become an orthopedic or trauma surgeon. I grew up in South Africa, so I witnessed some events which Europeans have a rather abstract understanding of. I wanted to help people right on the site. The musculoskeletal system fascinated me. To put it simply, the most interesting part and the driving force for me was helping injured or disabled people to regain their physical abilities, to again, or for the first time in their lives, become mobile and independent. This was the main reason for me to choose this specialty.
There are subspecialties within a broader specialty. The field of orthopedics, trauma, and hand surgery is extremely vast; it covers the entire musculoskeletal system from the upper vertebra to the toes. Providing high-quality medical care today requires more than a single orthopedic and trauma surgeon who can do everything. There are subspecialties (e.g., joint replacement, hand or back surgery) in which doctors train and perfect their skills so that they become experts. Of course, experience also matters. A doctor that time and again deals with certain clinical pictures, accumulates rich experience in the area. They are able to understand what it is exactly that the patient needs when conservative treatment methods have been exhausted and a surgery needs to be done. In this case, they have the expertise to recommend the most appropriate type of surgery. They say nothing beats experience. It is true for this medical field as well. The more you specialize, the faster you gain experience.
There is a range of options for each spine region treatment. But sometimes a surgery is the only option. A surgery is a procedure with fixed and practical routine. And bacterial inflammation, tumors, or fractures with nerve compression require a surgery without question. It’s more complicated with the so-called degenerative changes, for which options range from no treatment and simply comforting the patient to sometimes a very difficult surgery. You have to be really careful here. Textbooks rightly tell you that before going for a surgery, it is necessary to exhaust all nonoperative treatment options for a number of reasons:
First of all, humans have an innate ability to heal on their own, which should not be overlooked.
The second reason is that often not every nonoperative treatment method has been tried. A surgery should be considered only when you’ve run out of other options. Now let’s go back to the subspecialty topic. For example, a doctor that deals with back problems is able to perform the whole range of treatments and can also give recommendations. Of course, our experience allows us to understand when there are still nonoperative treatments worth trying and when a surgery is the best option.
The more alternatives there are, the more critically you need to think and the more critically you need to consider the necessity of a surgery.
Every year, several hundred patients stay at the hospital for nonsurgical treatment and more than a thousand for a surgery. Sometimes the first leads to the second. When dealing with changes due to wear and tear of the body, first we use infiltration treatment, facet thermocoagulation, endoscopic denervation, or SpineMED (spinal decompression) treatment. All these methods are appropriate for more conservative or at least minimally invasive pain management therapy.
For some patients, this kind of treatment isn’t enough, and they still need a surgery. There is a whole range of different surgeries, from decompression surgery used to treat compressed nerves to many-hours-long really complicated spine-straightening surgery, during which we correct the axis of the entire spine, partially or completely remove some vertebrae, and free considerable stretches of the spinal canal. The range of treatment methods is extremely wide. And it’s great that we are able to perform procedures such as imaging, intraoperative neuromonitoring, or intraoperative imaging here at Helios. We also have very experienced anesthesiologists and ICU doctors. Caring for patients who undergo surgery is a real team effort. Our hospital provides a variety of health care services even for the most seriously ill patients, which is not a given in every hospital.
A patient’s opinion plays a very important role, especially when it comes to back problems. The most important thing is what they want, what problems they have, and what outcome they expect. Communication with the patient before starting treatment is essential, among other things, for choosing an appropriate treatment method. So it’s always a shared decision, especially if it’s a surgery because there are risks and possible complications that a patient is subjected to. That’s why a thorough and detailed consultation before treatment is a must. A shared decision between patient and surgeon is fundamental for success.
Joint wear and tear or destruction (we do more than a thousand surgeries a year to fix this kind of issue), problems requiring orthopedic spine or pediatric surgery are the most common ones. Here in Krefeld, we have a large pediatric orthopedic center, led by our own specialist, and with leading departments of orthopedics/traumatology. Many patients come here for consultation or treatment from near and far.
Our other area of expertise is sports orthopedics. The surrounding region has a lot of sports clubs, which means a lot of sports injuries. And since we are the medical partner of the Rhine-Ruhr Olympic Training Center, very high level athletes (Bundesliga players, rowers, tennis players, horseback riders, etc.) come to our hospital. Every professional athlete that comes here with a sports injury wants and needs to get back to training as fast as possible.
Over the years, our hospital has grown and expanded significantly (Helios has three clinics only in Krefeld), and we have further developed subspecialties. One of our clinics has a large traumatology, pediatric orthopedics, spine and hand surgery department. In Hüls, we have an endoprosthetics department (knee and hip joints). The branch in Uerdingen—we call it the sports clinic—specializes in sports orthopedics and traumatology, as well as foot surgery. The subspecialization with different experts at different sites, who mainly work only in their own area of expertise, allows us to provide highly professional health care. This attracts patients from surrounding areas. Our development and subspecialization for the last decade made the hospital expand and brought us more local, national and foreign patients.
Most foreign patients come for arthroplasty (prosthesis), spine surgery, sports or pediatric orthopedic procedures.
Yes, I’ve had cases of prosthesis loosening or replacement surgery complications, as well as infections and complications after trauma treatment in other hospitals. In such situations, we have to do a revision surgery or come up with another treatment. Such cases are very frequent at our hospital.
That’s a good question. In all three branches, it’s about 5–10%, I think. Maybe even 15%. We have a lot of patients from the Netherlands.
Everything depends on the region. Communication among doctors in industrialized countries is on a high level. Large health centers in the U.S., Europe, and probably in Russia are on a similar level when it comes to what, when and where isomething should be done.
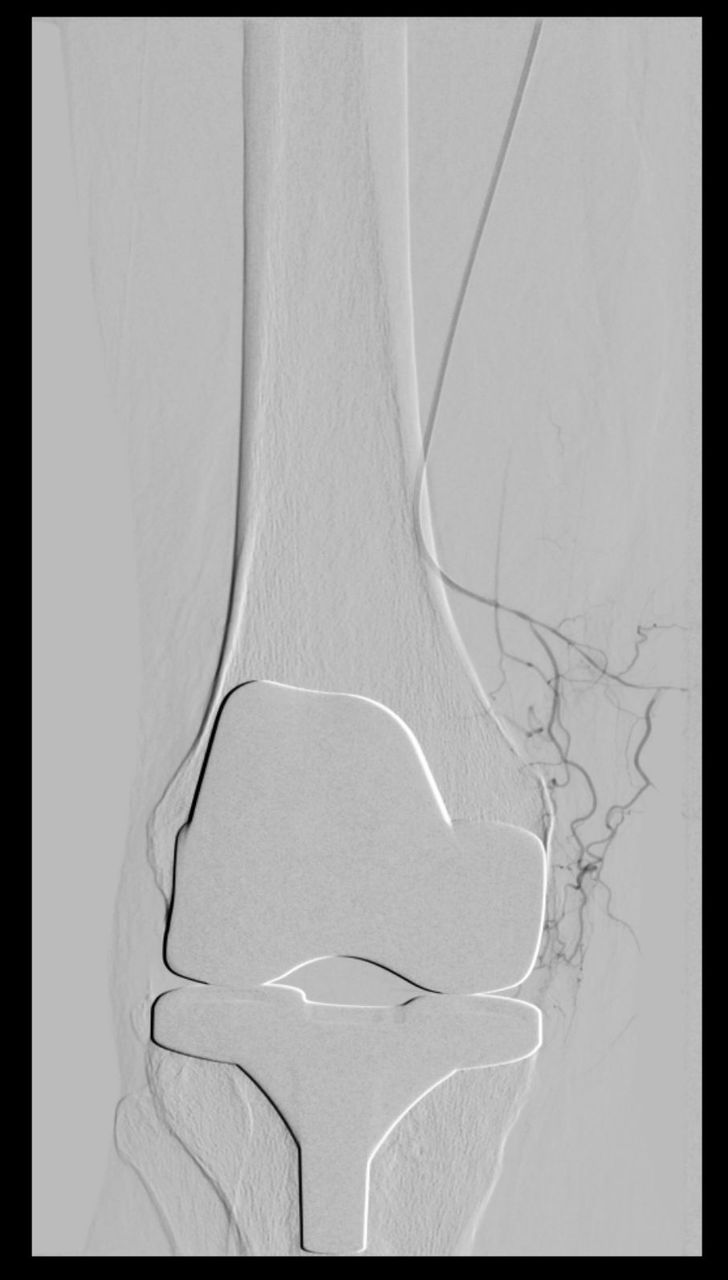
I think we all agree that if a patient has progressive osteoarthritis of the hip joint and severe pain, a hip arthroplasty is recommended. The road taken is generally the same. It is the type of prosthesis, materials, and fixation that can differ.
In Sweden, you would usually get a cemented prosthesis. If you get the surgery in the U.S., depending on the location, it would be a cemented or cementless endoprosthesis (often with a metal head). In Europe, especially in Germany, we use cementless endoprostheses when possible and, ideally, made of high-quality materials. It mainly depends on what the country’s healthcare system as a whole can provide. The situation in Germany is quite good. We can afford good and tested prostheses. We don’t have to choose between second- or third-class endoprostheses regardless of the patient’s insurance. However, not every country has such favorable circumstances. I believe the medical principles of what and when to do something are now the same in almost all industrialized countries. But it mainly depends on the country’s economic situation and what the government can and wants to do for its people. Here in Germany, we have the highest-level medical care.
"In Europe, especially in Germany, we use cementless endoprostheses."
Prof. Dr. Med. Clayton Kraft, head of the clinic for orthopedics, trauma, and hand surgery at Helios Hospital Krefeld
At Helios, especially in Krefeld, we use exclusive modern top-performance endoprostheses that last a long time. As for the technologies, we have the great opportunity to use robotics and individual templates for patients. We can also offer very individualized care. For example, we use minimally-invasive direct anterior approach (DAA) for hip arthroplasty. Not all Helios branches offer this type of treatment, but all do offer above-average care.
AMIS© (Anterior Minimal Invasive Surgery) is just a way of accessing the hip joint. It is also called DAA (Direct Anterior Approach). This minimally-invasive method is the standard we always apply. We use this approach for every hip arthroplasty, at least here in Krefeld. The only exception is when there is a fundamental reason that doesn’t allow us to do it. Although such cases are rare.
I personally only do hip and knee arthroplasty and all types of spine surgeries. If you need a shoulder arthroplasty, you can get it done in our hospital, but it would be performed by another doctor who specializes in shoulder surgery. This is the subspecialization that we talked about. We’ve had very good experience using it. A surgery should be performed by the one who can do it best, not only by the chief physician. The key concepts of our philosophy are quality and good results.
We frequently work with neurologists when treating patients with back problems because in such cases, we often have questions related to neurological aspects as well. Of course we work closely with anesthesiologists, ICU doctors, and cardiologists. Many surgeries we perform are completely elective, i.e., non-emergency surgeries we can carefully plan. We have a great responsibility to ensure that the patient undergoes such an operation safely despite all possible risks and complications. We carefully do our “homework” before the procedure, which often includes cardiological assessments and adjustments so that we can safely do everything our patient needs.
There is nothing wrong with the concept itself. This approach is still successfully applied in many countries (including Germany) and has been successfully used in many Helios hospitals for decades. But when we talk about what can be improved, we can add the concept of "all in one hand". It means that a single team cares for a patient, starting from admission to acute care treatment for hip or knee surgery up until discharge from a rehabilitation center. The core team consists of a surgeon and physiotherapists. This kind of close cooperation among different professionals allows to provide a patient with proper support so that they have to deal with almost no uncertainties during and after surgery.
In the past, when patients used to be transferred to another rehabilitation facility, there would always be uncertainties and problems. For example, a patient has a surgery and after 5–6 days, gets transferred to an external rehabilitation facility. And suddenly there is a swelling. The patient starts to worry and becomes anxious. They consult with the hospital where the surgery was done to check if there is nothing to worry about. So the patient is somewhere in between these unclear results, which is unsettling.
Nowadays, we follow a different procedure. Let's talk about an unusual course - We’ll use the same example of swelling of the leg. When this happens, the rehabilitation center sends for the surgeon who can assess the situation because they know the case and can promptly come to a conclusion and decide on the road map. The simple fact that the surgeon is readily available calms the patient and makes them confident.
It’s the same with physiotherapy. Physiotherapists are in attendance from the day of the surgery to discharge from the rehabilitation center. This means they know about everything that happens to the patient during and after the operation. All of this builds up great confidence and the patient understands that the whole team speaks the same language.
This is a very successful concept. The demand for a one-stop shop medical care is very high. Sometimes we even run out of beds in our rehabilitation center.
Yes, our hospital is among the first ones in Germany.
It’s a fairly new approach and we noticed that more and more hospitals copy it because of its success. A lot of patients come to our hospital for this very reason. This approach, along with our innovations in endoprosthetics, is one of the main reasons why patients choose us for surgical treatment.
This approach also includes fast-track recovery, doesn’t it? Could you tell us about it?
Sure. When a patient comes to get an arthroplasty done, we make sure they understand that they are not ill—they just need to get a certain part replaced. From the very start, we don’t let them fall into this kind of hospital mood. We have changed the old routines. You don’t need to fast prior to the surgery, and afterwards, you can eat and drink again very soon. We don’t use catheters. As for physical mobility, we tell our patients, “We operate in the morning, and in the afternoon, you get up.” And that’s what we do. Everything goes perfectly. The day after surgery, the patient can already move around their hospital room, and on the following day—the whole floor. If everything goes as planned, after about 3–4 days, the “acute” part ends. Next stop is the rehabilitation center. This approach works very well.
Before the surgery, we tell our patients that we’d like to see them being able to stand 1–2 hours after the surgery, in postanesthesia care unit if possible. This means that most patient take their first steps on the surgery day. On the second day, they are able to walk in front of their room with the help of their physiotherapist, and later on—use the stairs. We have a remobilization plan for these patients.
One of the success factors of our work is that patients know in advance what will happen to them. They know for sure that immediately after the surgery, someone will come and help them get back on their feet and that the orders come from their doctor. The fast-track recovery approach also implies that a physiotherapist comes to work with the patient already in the postanesthesia care unit, and this kind of work is not done by a nurse. We find this approach extremely successful.
"One of the success factors of our work is that patients know in advance what will happen to them."
We don’t expect the impossible. When the patient is old or feeble, the fast-track recovery is not going to work. But 80% of our patients can and want to take this approach. When possible, we guide our patients through pre-rehabilitation, i.e., prepare them and their family for what awaits them. This way they get to know how to use orthopedic products, what their new joint can withstand, and what they should avoid. If the patient is well informed in advance, it isn’t that difficult to inspire them to take such an innovative approach. After all, it’s about their own health.
There is a hospital exclusively for arthroplasty. Only endoprosthetic surgeries are done there. Everything there is about artificial joints. Everyone there understands the topic, and you can get all the answers.
Every day, 6 to 10 arthroplasties are done in an operating room, so all the surgeons and surgical nurses are immensely skilled in these procedures. As a result, we have standardized and routine operations. You can be sure that the people who do something frequently are really reliable and can provide very high-quality performance.
The orthopedic campus and rehabilitation center are on the same territory (the center is part of the building). Both of them are well equipped. They are spacious, the rooms are beautiful, and there is plenty of room to move around. It’s all about endoprosthetics, and the patients, who have different problems, feel this.
Time and again, foreign patients, who have been told that there was nothing else to be done to help them or that the surgery was too complicated, come to us.
I recall a patient from Russia who came to me about a year or a year and a half ago. He had been suffering from bilateral high hip dislocation since childhood. He’d been able to walk, but for several years before the surgery, it’d become progressively worse due to the destruction of the femoral heads.
We performed bilateral hip arthroplasty. These are more difficult operations because all muscles and tendons have to be lengthened. A doctor needs to very carefully prepare for this kind of surgery. But we were able to help this patient! Not long ago, he sent me a video of him walking. Knowing that he had been wheelchair bound when he came to me, naturally, I was very happy.
About six months ago, we had a patient from Bahrain. She had already had several preliminary surgeries in London. The damage to her right hip joint was significant. As a result of numerous surgeries, the prosthesis loosened. We fitted her with a hip prosthesis, replacing the entire femur and pelvis piece by piece. This helped her a lot.
So as you can see, we have some great stories of providing excellent care to patients. But I think every doctor can tell you such stories.
I think people have many fears and uncertainties about back surgery. I understand them because, of course, every one of us has a friend or relative who underwent back surgery and was not happy with it at all.
This often happens due to incorrect indications determining. Meaning that the patient shouldn’t have been operated at all or they should have had another kind of surgery. Unfortunately, this leads to unsatisfactory results in patients who have had “partial” surgeries several times. This also leads to the whole topic of spinal surgery being incredibly discredited. So there’s some skepticism, and people say, “Don’t get the surgery. Smith had the same one. He’s much worse now.” You can’t make such stories disappear. Besides, you have to agree to some extent because this does happen sometimes. But fundamentally, surgical spine treatment is wrongly condemned. With proper indications assessment and correctly performed operations, the results are good. Unfortunately, in comparison to the “bad” ones, the happy-end stories are not heard at all or very rarely. Patients who are truly happy with the result often say, “If I’d known earlier, I’d have it done a long time ago.”
Recognizing indications correctly and ordering right treatment are certainly a great gift when it comes to back surgery, which helps you make the lion’s share of your patients ultimately satisfied. But breaking the ice and getting rid of the fear is sometimes quite difficult.
As for the first question, there are some obvious symptoms that don’t require immediate treatment. For example, sporadic back pain that goes away on its own. When the patient says that it’s mild and happens only every two years. The same goes for nonspecific back pain that anyone can experience. But when there is a combination of symptoms, namely, unbearable back pain, stiffness, poor response to painkillers, pain radiating to the legs, neurological symptoms or weight loss, fever, chills, disturbed night sleep—all of this must be looked into until it’s clear that there’s nothing more serious behind it.
As for the question about joint degeneration, indeed, if a patient experiences pain or if the mobility is generally still quite satisfactory and pain occurs only from time to time, the patient should first undergo a course of conservative therapy.
But when an X-ray shows significant bone destruction, pain is already significant, conservative therapies are no longer sufficient, and the patient can no longer cope, it’s time to think about a surgery.
And of course, the third factor is age. The younger the patient, the more critically you need to approach the question of surgery. When talking about joint replacement surgery, we need to think carefully about preserving options.
I chose it because it’s a large hospital and I can treat an incredibly wide range of patients here. I have a great team and amazingly good medical and nonmedical staff with a wide range of expertise here. We discuss various issues quite openly. If I have a question or I’m not sure which medical decision is better, I have at least two or three colleagues with whom I can discuss these issues. We can exchange thoughts and ideas. “What can we do in this case? What would be rational? And what wouldn’t?” It’s a great pleasure to work with such a large and versatile team of very intelligent people. Not everyone is that lucky.
I am the head of the orthopedics/traumatology section. We have five working groups with different specializations. Within a group, doctors who specialize in the same area are brought together.
For example, doctors who work in trauma and emergency surgery meet there and exchange not only their experiences but also the latest developments in the field. They discuss endoprosthesis materials, new products on the market, obsolete materials, standards changes or the need to introduce new standards. All of these influence the whole section, the whole working group, which means that we always try to be at the forefront of medicine here at Helios. Many things change in a relatively short time, so it’s extremely important to stay up to date and be aware of the direction the modern medicine is taking and where we, as an orthopedic/accident surgery group, want to be.
"We always try to be at the forefront of medicine here at Helios."
I think there are two big areas that are going to develop even faster over the course of the next 5–10 years. The first one is robotics. We already use robots at four Helios clinics. Some of them assist us during endoprosthetic surgeries.
And the second is imaging (including interoperative imaging). It helps us place endoprostheses, osteosynthesis devices, and spinal implants even more accurately.
I believe these technological developments will have a significant impact on our field in the coming years and, eventually, will aid us to achieve even better quality of medical care.
Read more:
Do you need more information about Helios Hospitals or want to schedule your treatment?